Max Hospital, Patparganj, New Delhi
Elevate Health Solutions, Rajouri Garden, New Delhi
Max Hospital, Vaishali, Ghaziabad
Max Hospital, Patparganj, New Delhi
Elevate Health Solutions, Rajouri Garden, New Delhi
Max Hospital, Vaishali, Ghaziabad

08 Mar, 2022
Most common symptom of food pipe cancer is difficulty in swallowing. Initially, there may be just some difficulty in swallowing (medically called dysphagia) of solid food which gradually progresses to inability to swallow even liquids. Inability to take oral diet may result in weight loss. Symptoms of more advanced disease include hoarseness of voice, decreased appetite (medically called anorexia), cough on swallowing, and even later bone pains, headache and jaundice. Food pipe cancer more often manifests as gradually worsening difficulty in swallowing (compared to a sudden onset problem which would be more often due to a stuck food bolus/foreign body).
One should consult a doctor preferably a gastrointestinal (GI) surgeon or a gastroenterologist who would, after a thorough clinical evaluation, advise an upper GI endoscopy at which the tumour would be seen along with its starting location in food pipe, distal extent as well as the degree of luminal narrowing. A biopsy would also be taken at this point to confirm the presence of cancer. If there is significant difficulty in swallowing, it helps if a Ryle’s tube is placed at this point at endoscopy to ensure patient can get the required nutrition. Ryle’ stube is a thin tube placed through the nose with its tip in the stomach through which feeds can be given to the patient easily by the attendants even at home. This would usually be followed by a PET-CT which would help confirm the extent (stage) of disease. Most patients have locoregional (advanced) disease at diagnosis and the disease has not spread to distant organs (metastatic disease). Occasionally, the disease may be diagnosed at an early stage, wherein the doctor may advice an endoscopic ultrasound to confirm that the disease is very localized (or early stage).
Treatment is guided by patient condition (most importantly what the patient can do in daily life at the time of diagnosis), extent of disease and location of tumour.
It is important to ensure an adequate nutrition, cessation of smoking and alcohol if applicable, deep breathing exercises spirometry and brisk walking to help keep the chest in good condition. Careful attention needs to be given to co-existing illnesses including but not limited to diabetes, hypertension, cardiac or pulmonary diseases and ensure that these are optimally attended to.
Unfortunately, most patients present at a more advanced stage wherein they would be treated with multimodality treatment comprising chemotherapy, radiotherapy and surgery. Tumors located in early part of food pipe (proximal oesophagus) would be treated by a combination of chemotherapy and radiotherapy (definitive chemoradiation) which is quite effective with surgery being deemed largely not advisable. Patients with Stage IV (also called metastatic disease meaning disease which has spread to other parts of body) would be treated based on symptoms and extent of disease. Patients who are unable to take orally are initially treated with endoscopic SEMS placement (metal stent placed endoscopically across the tumour) to enable them to swallow food. Sometimes, patients have significantly reduced appetite, in which case placement of additional Ryle’s tube through the stent (as also mentioned in early evaluation) for supplemental feeding. Subsequently, patients would be treated with chemotherapy with/without radiotherapy.
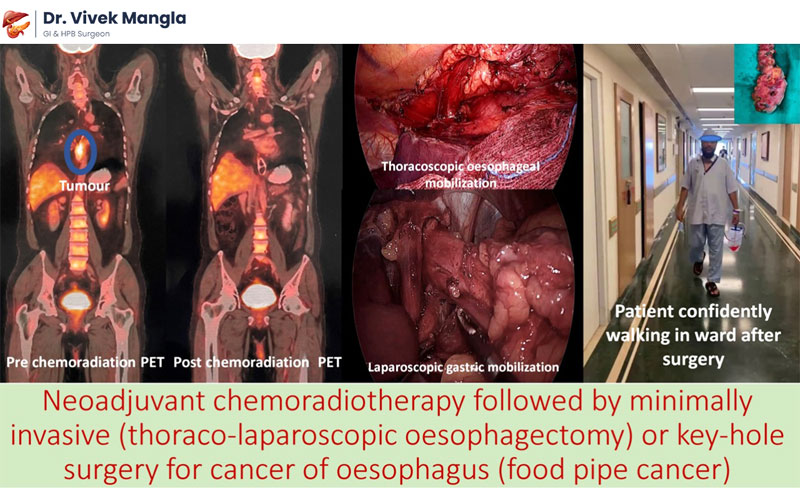
Most patients with tumours in mid and distal thirds of food pipe would be treated initially with chemoradiation and sometimes chemotherapy alone followed by surgery (as mentioned above). Radiotherapy would be given in 23 small doses (called fractions) (usually 5 days a week; over 4.5 weeks). This would be combined with a small dose of chemotherapy given one day in a week (a total of 5 doses, preferably a combination of two drugs if permitted by patient’s condition). This would be followed by an assessment of response to treatment about 4-6 weeks after completion of radiation with a repeat PET-CT scan and most likely surgery. Most patients have a very good response to chemoradiation, and the tumour may not be visible on the repeat PET-CT. evidence available today suggests that most such patients would have residual tumour in the food pipe which may not be visible on PET CT and even endoscopy and hence should undergo surgery unless the patient has significant comorbid illnesses precluding surgery.
Occasionally, when the disease is diagnosed at a very early-stage disease, it may, in this situation, be treated by endoscopy (for precancerous lesions) and surgery directly.
Surgery entails removal of a part or whole of food pipe with surrounding lymph nodes (both in the chest and abdomen) and its substitution by either the stomach (most commonly) or a part of the large intestine (colon) which is joined to the food pipe most often in the neck and sometimes in the chest depending on tumour location. This surgery conventionally done by open technique, is now done mostly by minimally invasive surgery (either thoracolaparoscopic or robotic techniques) with the benefit of faster and better recovery, lesser complications and better cosmesis with good long-term oncologic outcomes.

Most patients would be kept in ICU for observation for a day or sometimes more time depending on their recovery. There would be some tubes placed in chest/abdomen which would be removed over the next few days. Most patients would have a feeding access through which liquid feeds would be started from day 1-day 3 onwards depending on protocol of the treating institution. Importantly, the liquid feeds must be given slowly, about 200-300 ml over about 1-2 hours, at 3–4-hour interval as needed. The tube must be flushed with water about 50 ml slowly after each field to ensure that the particulate matter in the feed does not deposit in the tube and block it. It is important for the patient and family to learn care of the feeding tube and e comfortable with it as it helps avoid problems with its use later on at home when needed.
Minimally invasive surgery helps patient experience less pain, early ambulation, lesser wound related complications, lesser pulmonary complications, and faster recovery. Most patients would be discharged to home care between postoperative day 6-10, some patients with complications may need to stay longer. Most patients would be taking orally small amount food, with feeds supplementation and able to comfortably walk around and able to do activities of self-care at discharge.
After discharge, patients are encouraged to walk and do deep breathing exercises. Patients are advised to maintain a 30 degrees head end elevation when lying down. Gradually oral diet is increased as per tolerance, mostly a small amount orally at a time. Avoiding water at mealtime helps ensure that the patient takes soft diet, and the small residual stomach does not get filled up with water and patient is able to get adequate calories and protein in the diet. An upright posture for about half an hour after meals should be maintained. Feeding tube feeds would be continued till patient is able to take adequate amounts orally and reduced one this is achieved.
Surgery for food pipe cancer is a major surgery, and maybe associated with a few complications including but not limited to cardiorespiratory issues, persistent drainage in chest tube and sometimes leak from the place where the stomach is rejoined to the food pipe. With careful attention to detail intraoperatively and postoperatively, the treating team would be able to prevent and manage most of these. The incidence of these tends to be low, and most patients recover well and hence benefit from surgery. Overall risk to life would vary from 2-10% depending on risk factors such as cardiorespiratory status, exercise capacity and nutritional status etc.
Patients with adenocarcinoma of oesophagus would usually be offered adjuvant chemotherapy. Patients with squamous cell cancer would be offered either a follow up or a targeted therapy which is of some benefit albeit at a high economic cost. Follow up comprises a 3 monthly clinical examination, evaluation for symptoms, and a PET-CT to rule out disease recurrence in the 1st year. Frequency of tests/follow up can be reduced once time has elapsed since diagnosis/treatment.
Diagnosed timely and treated appropriately, most patients would benefit from treatment. A significant proportion of patients would be cured as well in absence of verry extensive disease. The 5-year survival (used as a surrogate marker for cure) with cancer located only in the food pipe is 47%. The 5-year survival rate for those with disease extending to surrounding tissues and/or regional lymph nodes is 25%. Survival rate for patients with distant spread is low (5%).